Blog
Blood vessel abnormalities in the attention could drive Alzheimer’s disease
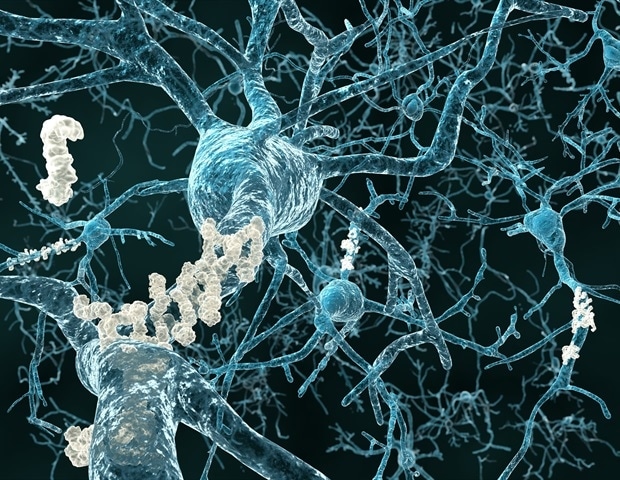
Blood vessel abnormalities in the attention are a significant component within the progression of Alzheimer’s disease, in keeping with research from Cedars-Sinai investigators published within the peer-reviewed journal Alzheimer’s & Dementia: The Journal of the Alzheimer’s Association. These changes correspond to changes within the brain, offering a brand new possibility for early diagnosis.
“This study provides a brand new understanding of the vascular changes related to Alzheimer’s disease, especially within the retina, the layer of nerve tissue behind the attention,” said Maya Koronyo-Hamaoui, PhD, professor of Neurology, Neurosurgery and Biomedical Sciences at Cedars-Sinai and senior writer of the study. “It also points to the damage Alzheimer’s disease causes to the blood vessels within the retina, enabling a brand new, noninvasive pathway to early diagnosis and monitoring of disease progression.”
Investigators compared blood vessels in retinas collected from 24 human donors with Alzheimer’s disease, 10 donors with mild cognitive impairment and 27 with normal cognition.
In patients with Alzheimer’s disease and mild cognitive impairment, they found certainly one of the earliest signs of Alzheimer’s disease so far: disruption of the blood-retinal barrier, where tightly joined cells prevent harmful substances from entering the retinal tissue.
“In patients with Alzheimer’s disease, we found that there was a deficit of as much as 70% in that barrier, meaning harmful substances can go through and enter the retinal tissue,” said Haoshen Shi, MD, PhD, project scientist and first writer of the study. “We see that this happens very early on, in patients with only mild functional impairment.”
Damage to the blood-retinal barrier was strongly related to a condition called cerebral amyloid angiopathy (CAA)-;the buildup of amyloid proteins in small blood vessels-;and other vascular disease within the brain.
“Currently, the one solution to detect CAA in patients is in post-mortem brain tissue samples,” said Koronyo-Hamaoui. “With additional research and the event of advanced retinal imaging, vascular and blood-retinal barrier damage could give us the primary opportunity to detect CAA in living patients.”
The study also found that deposits of a protein called amyloid beta 40 collected within the retinal arteries of Alzheimer’s disease patients, making the arteries stiff, disrupting blood flow and stopping the arteries from clearing harmful substances from the retina. Further studies are vital to find out whether the deposits accumulate due to blood vessel damage, or actually cause the damage, Koronyo-Hamaoui said.
“Retinal and brain tissues are wealthy in blood vessels, and high blood supply is key for his or her function,” Koronyo-Hamaoui said. “Restriction of blood supply, which can occur because of the damage we show happening here, implies that these cells don’t get the oxygen and the nutrients that they need.”
Advanced retinal imaging, which might take a look at the blood vessels and protein accumulation noninvasively in living patients, is in development but shouldn’t be yet approved by the Food and Drug Administration, Koronyo-Hamaoui said.
As an anatomical extension of the brain, the retina has been extensively examined as a window to central nervous system disorders. This work adds to recent progress in advanced retinal imaging and identification of other retinal biomarkers to advance the science of Alzheimer’s disease early detection.”
Keith L. Black, MD, Chair of the Department of Neurosurgery and the Ruth and Lawrence Harvey Chair in Neuroscience at Cedars-Sinai
Meanwhile, Koronyo-Hamaoui advises people to do what they’ll to maintain their circulatory system, including the blood vessels within the retina and the brain, healthy to assist prevent CAA and dementia.
“Controlling hypertension, eating a healthy weight-reduction plan low in sugar, reducing alcohol consumption and avoiding smoking helps prevent chronic inflammation and damage to blood vessels,” Koronyo-Hamaoui said. “Our study shows that blood vessel damage is a significant element within the progression of Alzheimer’s disease.”