Blog
Pulsed field ablation secure, effective for the treatment of paroxysmal atrial fibrillation
Pulsed field ablation (PFA) is as effective and secure as conventional thermal ablation for the treatment of paroxysmal atrial fibrillation (AF), in keeping with late breaking research presented in a Hot Line session today at ESC Congress 2023.
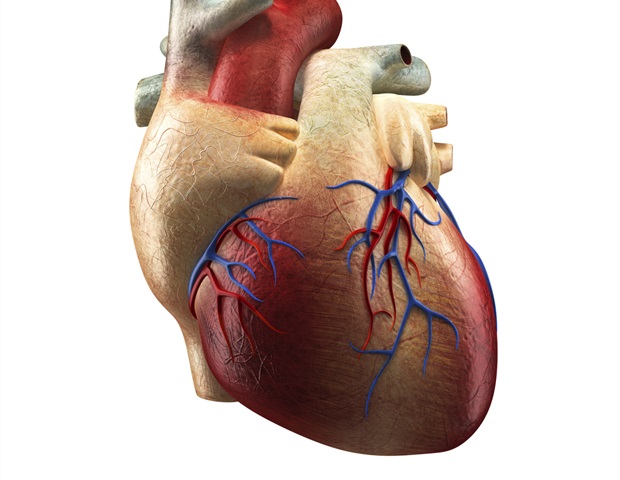
ESC guidelines recommend catheter ablation after failure of drug therapy in patients with paroxysmal AF.2 Conventional ablation technology uses thermal energy (either heat/radiofrequency energy or cold/cryothermal energy) to ablate the tissue. Unlike thermal ablation, PFA uses high energy electrical pulses to destroy tissue by a process called electroporation. Preclinical and clinical studies have demonstrated that PFA seems to preferentially ablate the center tissue, with minimal or no damage to surrounding structures reminiscent of the oesophagus and phrenic nerve, in addition to no pulmonary vein stenosis – all complications that may occur with conventional thermal ablation.3-6
ADVENT was the primary randomised controlled trial comparing PFA to traditional ablation (either radiofrequency or cryothermal ablation).7 The trial is meant to tell Food and Drug Administration (FDA) approval of the PFA catheter within the US. The study enrolled patients with drug-resistant, symptomatic paroxysmal AF. One to 3 roll-in patients were permitted at each site to make sure experience using the PFA catheter. The remaining patients were randomised in a 1:1 ratio to PFA or conventional thermal ablation. At the start of the trial, roughly 50% of centres were assigned to radiofrequency energy for the control group and the remaining centres were assigned to cryothermal energy for the control group. Patients were followed for 12 months with weekly electrocardiogram transmissions and 72-hour Holter assessments at six and 12 months.
A complete of 687 patients underwent ablation by 65 operators at 30 centres within the US. The initial roll-in phase included 80 patients; the remaining 607 patients were randomised to PFA (305 patients) or conventional thermal ablation (302 patients, of which 167 received radiofrequency ablation and 135 received cryoablation). The common age of randomised participants was 62 years and roughly 35% were female.
The first efficacy endpoint was the success rate, defined as acute success and chronic success (one-year freedom from recurrent atrial arrhythmias, antiarrhythmic drug use, and cardioversion or repeat ablation). The success rate was 73.3% and 71.3% within the PFA and thermal groups, respectively, and met the prespecified criteria for noninferiority (between-group difference, 2.0%; 95% Bayesian credible interval [BCI], -5.2 to 9.2%; posterior probability of noninferiority >0.999). The secondary efficacy endpoint was the identical as the first efficacy endpoint, but tested for superiority: this didn’t meet the standards for superiority (posterior probability of superiority 0.708).
The first safety endpoint was a composite of great antagonistic events related to make use of of an ablation catheter or the procedure itself and occurring inside seven days, in addition to pulmonary vein stenosis or oesophageal fistula occurring at any time in the course of the 12-month follow up. This endpoint occurred in 2.1% and 1.5% patients within the PFA and thermal groups, respectively, and met the prespecified criteria for noninferiority (between-group difference, 0.6%; 95% BCI, -1.5 to 2.8%; posterior probability of noninferiority >0.999). The secondary safety endpoint was the change in pulmonary vein dimension (i.e., any stenosis or narrowing) from baseline to day 90. The reductions in vein cross-sectional area were 3.3% and 19.5% within the PFA and thermal groups, respectively, which met the prespecified criteria for superiority of PFA (posterior probability of superiority >0.999).
The ADVENT trial showed that PFA is as effective and secure as conventional thermal ablation to treat paroxysmal AF. Procedure times were faster for PFA than thermal ablation, but there was more X-ray exposure with PFA.”
Vivek Reddy, Principal Investigator, Professor, Icahn School of Medicine at Mount Sinai, Recent York, US
Source: