Blog
Hospitals urged to adopt recent MRSA prevention strategies
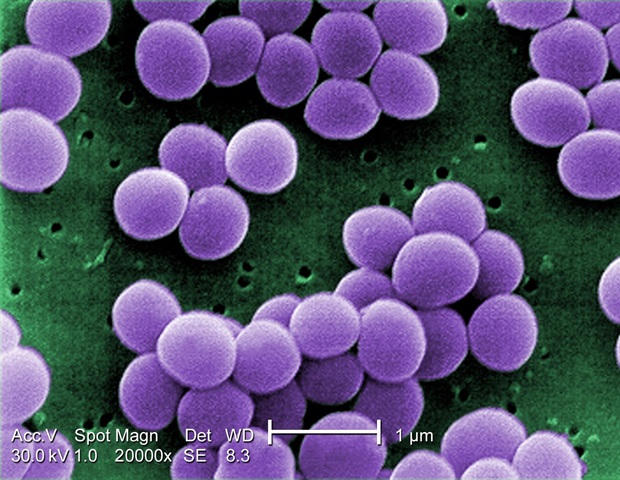
A bunch of 5 medical organizations have released updated recommendations for the prevention of methicillin-resistant Staphylococcus aureus, referred to as MRSA, transmission and infection. MRSA causes roughly 10% of hospital-associated infections in the US and such infections are related to an increased risk of death. Certain infections brought on by MRSA rose by as much as 41% throughout the pandemic after falling in preceding years.
Strategies to Prevent Methicillin-Resistant Staphylococcus aureus Transmission and Infection in Acute Care Hospitals provides evidence-based, practical recommendations to stop the spread of MRSA and reduce the chance of MRSA infection. The document, published today within the journal Infection Control & Hospital Epidemiology, is probably the most recently updated guidance within the series known collectively because the Compendium.
The large strain placed on healthcare throughout the pandemic could have contributed to the observed increase in some hospital infections. We now have data that show MRSA infections rose. The evidence that informs these recommendations shows that we will be successful in stopping transmission and infection. We will get back to the pre-2020 rates after which do even higher.”
David Calfee, Study Senior Writer and Editor, ICHE, Society for Healthcare Epidemiology of America
The updated recommendations elevate antimicrobial stewardship – an effort focused on improving how antibiotics are prescribed and used – from an “additional practice” to an “essential practice,” meaning all hospitals should do it. When someone who’s colonized with MRSA receives treatment with antibiotics for an additional infection, they could have a better risk of developing MRSA infection and will be more more likely to transmit MRSA to others. Avoiding unnecessary use of antibiotics may decrease these and other risks related to antibiotic use, corresponding to C. difficile infection.
The guidance describes other practices -; surveillance to detect asymptomatic MRSA carriers and decolonization to eradicate or reduce the burden MRSA amongst people who find themselves colonized with MRSA -; for specific patient populations.
“Basic infection prevention practices, corresponding to hand hygiene and cleansing and disinfection of the healthcare environment and equipment, remain foundational for stopping MRSA,” Calfee said. “These fundamental practices help to stop the spread of other pathogens as well.”
The authors retained contact precautions, using a gown and gloves when providing care to a patient with MRSA colonization or infection, as a vital practice. Nonetheless, the authors acknowledge that for quite a lot of reasons some hospitals have chosen to change or could also be considering modification of using contact precautions for all or some patients who’re colonized or infected with MRSA. The updated recommendations provide guidance to assist such hospitals assess risk, make informed decisions, monitor outcomes related to changes in using contact precautions, and discover populations and scenarios during which continued use of contact precautions must be considered.
MRSA infection is brought on by a form of staph bacteria that’s proof against lots of the antibiotics used to treat bizarre staph infections. Healthcare-associated MRSA infections often follow invasive procedures, corresponding to surgeries, or using devices, corresponding to central venous catheters, and will be spread inside hospitals by the hands of health care personnel or through contact with contaminated surfaces and equipment.
The guidance updates the 2014 Strategies to Prevent Methicillin-Resistant Staphylococcus aureus Transmission and Infection in Acute Care Hospitals. The Compendium, first published in 2008, is sponsored by the Society for Healthcare Epidemiology (SHEA). It’s the product of a collaborative effort led by SHEA, with the Infectious Diseases Society of America, the Association for Professionals in Infection Control and Epidemiology, the American Hospital Association, and The Joint Commission, with major contributions from representatives of several organizations and societies with content expertise. The Compendium is a multiyear, highly collaborative guidance-writing effort by over 100 experts from around the globe.
In coming weeks, a brand new Compendium section will likely be published outlining approaches to implementation of infection prevention strategies, followed by an update to strategies to stop catheter-associated urinary tract infections.
Recently published Compendium updates include strategies for stopping surgical site infections, central line-associated bloodstream infections, ventilator and non-ventilator associated pneumonia and events, C. difficile infection, and techniques to stop healthcare-associated infections through hand hygiene.
Each Compendium article accommodates infection prevention strategies, performance measures, and approaches to implementation. Compendium recommendations are derived from a synthesis of systematic literature review, evaluation of the evidence, practical and implementation-based considerations, and expert consensus.